 Download this patient information sheet
Download this patient information sheet
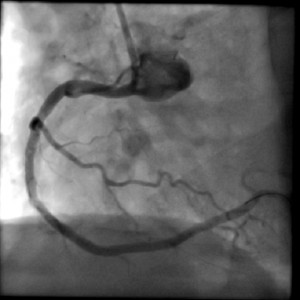
Coronary stenting is often used instead of surgery to open up narrowed or blocked coronary arteries. It is done in hospital in the catheter laboratory in much the same way as a coronary angiogram.
Coronary stenting is performed to open up narrowed or blocked coronary arteries. This is usually to try to improve symptoms of chest pain, shortness of breath or other difficulties. Coronary stenting may also be performed as an urgent procedure to avert a heart attack
After an injection of local anaesthetic, a fine tube (catheter) is put into the artery in the groin or from the wrist. The tube is carefully passed into the affected part of the artery using x-ray guidance. A tiny wire is passed down the artery so that a sausage shaped balloon can be passed over it and into the part that is narrowed or blocked.
To open up the artery, the balloon is blow up with fluid, which then presses against the material blocking the artery, pushing it out of the way. A stent – a fine metal tube sleeve or spring coil – is passed into the diseased part of the artery using a balloon. The balloon is removed once the stent is in place.
The stent stays in for life. After the procedure, you will be given some medications which reduce your risk of blood clotting and blocking the stents.
Clopidogrel or other blood thinning drugs are used for several months and often longer. A small daily dose of aspirin may need to be taken for the rest of your life.
The procedure is usually done using local anaesthetic to numb the area. If you have any concerns, talk these over with your doctor.
Yes. Your cardiologist will usually be the person suggesting you undergo coronary stenting, usually after having performed other tests, including a coronary angiogram. You will need to have a blood test a few days before the test. You will be fasting (no breakfast or drink) on the morning of the test. You will have tell your cardiologist if you have had a contrast (x-ray dye) reaction before; in this case, special precautions are needed. Your cardiologist may instruct you to take certain blood thinning drugs in preparation for a coronary angiogram, and in general you should continue all your usual pills, unless instructed otherwise.
As you might expect with a procedure that involves placing something in the body and stretching an artery open, there are small risks associated with coronary stenting. These risks depend on
The risks below are a guide to some of the more serious risks that can happen. These are not the only risks
Less than 1 in 10,000 people:
Less than 1 in 1000 people:
Less than 4 in 1000 people:
Less than 1 in 100 people:
Less than 1 in 20 people:
Less than 1 in 10 to 1 in 20 people:
There are special types of stents (known as drug eluting stents) that can stop the artery from narrowing again. These stents are successful for 95 out of a 100 people but their use depends on the type of narrowing and a number of factors related to the patient.